Resources
Practice
More >
Talks & Articles
More >
– Awareness of Breathing –
Practice Instructions
– Loving Kindness Meditation –
Practice Instructions
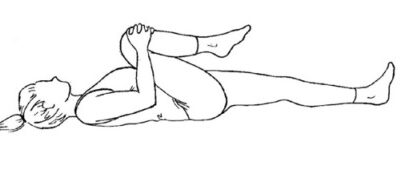
– Mindful Movement with Gentle Yoga –
Instructions and Diagrams for Practice
– The Body Scan –
Practice Instructions
A Note on Noting
Practice suggestions from Stephen Levine
Affectionate Breath and Finding Joy
Teresa Johnson - 21 minute audio
Affectionate Breathing
Tim Burnett - 24 minute audio
Affectionate Breathing Meditation
Carolyn McCarthy - 20 minute audio
Affectionate Breathing Meditation
Catherine Duffy - 19 minute audio
Anchoring Meditation
Carolyn McCarthy - 8 minute video
Anchoring Meditation
Tim Burnett - 22 minute audio
Awareness of Breathing
Catherine Duffy - 20 minute audio
Awareness of Breathing
Tim Burnett - 5 minute video
Awareness of Breathing
Tim Burnett - 22 minute audio
Awareness of Breathing
Teresa Johnson - 25 minute audio
Awareness of Breathing
Beth Glosten - 20 minute audio
Balancing Groundedness & Openness
Tim Burnett - 34 minute audio
Benefits of Loving Kindness
An article from Mindful Magazine
October 2014
Beyond Utility Meditation
Tim Burnett - 40 minute audio
Body Scan
Catherine Duffy - 30 minute audio
Poetry Index
By connecting us to emotion, intuition, and the unknown, poetry contributes to the rich, mysterious fabric of a multi-layered mindfulness experience. Here are a few of our favorites. We encourage you to seek out these poems and poets.
David Budbill ~ Bugs in a Bowl
Lucille Clifton ~ Blessing the Boats
Billy Collins ~ Aimless Love
Dana Faulds ~ Allow
Hafiz ~ Admit Something
Tony Hoagland ~ The Word
Sister Dang Nhiem ~ Feather at Midday
Mary Oliver ~ The Summer’s Day, Mindful
Portia Nelson ~ Autobiography in Five Chapters
Kaveri Patel ~ Dear You
Rumi ~ The Guest House
May Sarton ~ Beyond the Question, 1
Naomi Shihab Nye ~ Shoulders, Kindness
Rosemerry Trommer ~ One Morning
Derek Walcott ~ Love After Love
John Welwood ~ Forget About Enlightenment